Spike Protein Basics
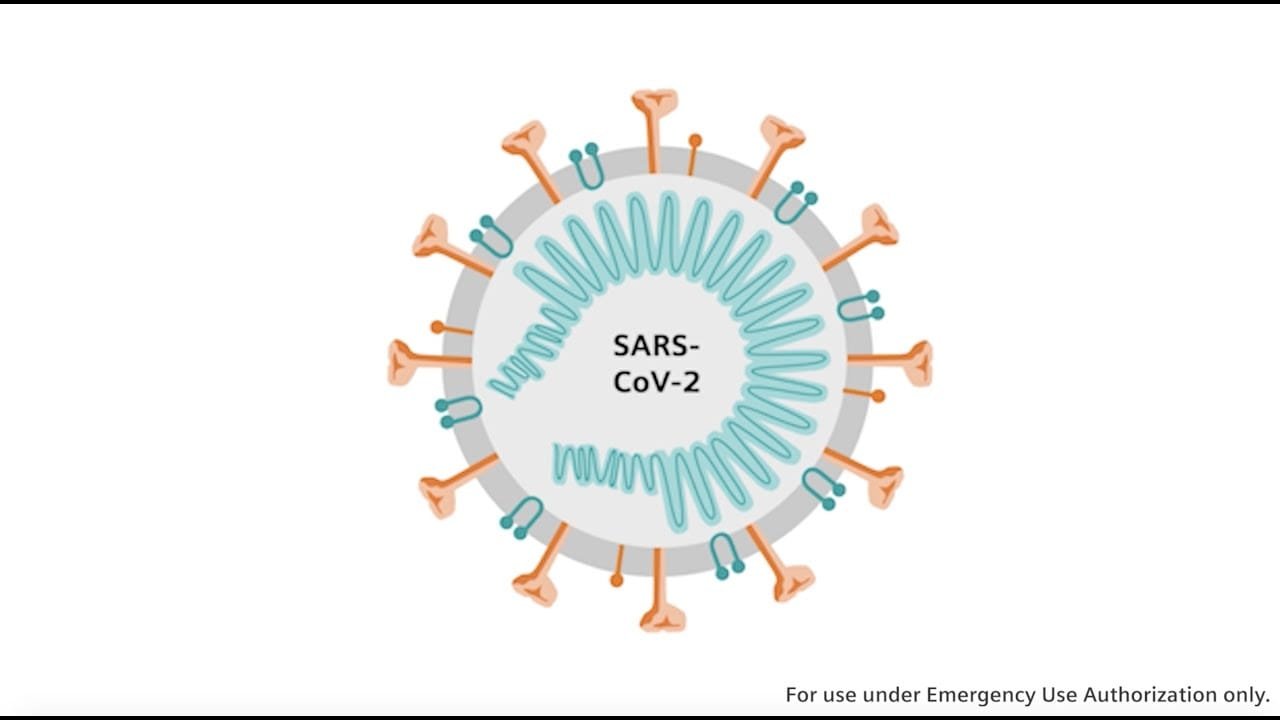
Spike proteins are like the keys that allow viruses, and specifically the novel coronavirus, to unlock the doorway into a host cell. These proteins are not just a characteristic feature of coronaviruses such as SARS-CoV-2, the virus responsible for COVID-19; they’re a critical part of its anatomy that enables it to hijack a cell’s machinery for its own viral reproduction.
The spike protein binds to the host cell’s receptor, known as angiotensin-converting enzyme 2 (ACE2), which triggers the virus’s entry into the cell. Once inside, the virus releases its RNA, starting the viral lifecycle and ultimately the production of more viral particles which can go on to infect other cells.
These spike proteins are not static; they undergo a change in structure from what is known as the prefusion to the postfusion conformation. Such transitions are crucial in the context of viral binding and fusion with the cellular membrane of the host cell.
| Function | Description |
|---|---|
| Binding | Spike proteins attach to ACE2 on the host cell surface. |
| Fusion | They enable the merging of viral and cellular membranes. |
| Immune Recognition | They are target sites for the host’s immune response. |
When the body encounters these spike proteins through a vaccine or natural infection, it generates an immune response, effectively teaching the immune system to recognize and combat the pathogen.
Moreover, it’s fascinating to note that the spike protein and its receptor-binding domains are a focus of intense research for the development of treatments and vaccines since they are the primary interface between the virus and human cells.
From a scientific perspective, understanding spike proteins is a window into understanding the viral life cycle and how to disrupt it, ultimately helping to curb the spread of not only COVID-19 but also other diseases caused by similar pathogens.
Spike Protein and Immunity

Investigating the role of the spike protein provides crucial insights into how vaccines rally antibodies to our defense and how mutations can change the game in the Covid-19 pandemic. It’s a microscopic arms race where the immune system and the virus constantly evolve.
Antibodies and Vaccines
The spike protein of SARS-CoV-2 is the main target for antibody responses post vaccination. Covid-19 vaccines such as those developed by Pfizer and Moderna use modified messenger RNA (mRNA) to teach muscle cells to create a version of the spike protein. This, in turn, triggers an immune response and fosters the production of neutralizing antibodies—essentially preparing our immune system for future encounters with the virus.
Mutation and Variants
Viruses are wily foes, and the spike protein is no exception when it comes to mutations. As the virus replicates, changes in the spike protein can result in variants, like those first identified in the UK, South Africa, and Brazil, which can be more efficient at viral entry into human cells. The S1 and S2 subunits of the spike protein, along with its receptor-binding domain (RBD), are often the hotspots for these mutations, potentially affecting the virus’s ability to infect and the effectiveness of vaccines.
T Cells and the Cellular Response
While antibodies often steal the spotlight, T cells also play a critical role in the cellular response to SARS-CoV-2’s spike protein. They seek out and destroy infected host cells, preventing further viral replication. T cells can recognize and respond to fragments of the spike protein presented on the surface of infected cells, providing another layer of protection against Covid-19.
Global Health Impact
Covid-19 vaccines like Novavax, which includes a lab-made version of the spike protein, or those using adenovirus vectors, have significantly impacted global health. By priming the immune response without causing disease, they have proved a crucial tool in curbing the pandemic’s tide. These vaccines have underscored the spike protein’s central role in driving immunity and paved the way for innovations in vaccine technology.
To explore the intricate dance between the immune system and the spike protein can, take a peek at the detailed analysis of “vaccine-induced immune imprinting” and the structural insights into the “glycan shield on the spike protein”, which have broad implications for our understanding of immune recognition.
Advances in Research and Treatment

Recent scientific efforts have led to significant breakthroughs in the understanding and treatment of virus-related illnesses, particularly by targeting the spike proteins of viruses such as SARS-CoV-2.
Clinical and Therapeutic Developments
Researchers have developed an antibody cocktail that, by targeting the SARS-CoV-2 spike protein, prevents the virus from escaping treatment that might occur with individual antibodies. This kind of treatment provides a therapeutic solution that remains effective against various mutations of the virus. Simultaneously, vaccines have employed the use of spike proteins to induce immunity in individuals, essentially training the immune system to recognize and combat the virus.
Understanding on a Molecular Level
Studies involving SARS-CoV-2 have been greatly aided by techniques like cryo-electron microscopy, allowing researchers to examine the virus at an atomic level. Insights into how the spike protein is glycosylated and how it interacts with human cells have been pivotal. For instance, understanding the spike protein’s amino acid composition and domains can lead to new therapeutic approaches.
Potential for Future Pandemics
The knowledge garnered from studying SARS-CoV-2’s spike protein provides crucial groundwork for dealing with future pandemics. Whether facing a new strain of influenza virus, coronaviruses like SARS or Middle East Respiratory Syndrome, or unrelated pathogens like Ebola, the principles of how to tackle a highly transmissible virus at a molecular level are becoming clearer. Advances in neutralizing antibodies can now be used as a platform for developing treatments against a variety of viral threats.