Understanding Vagus Nerve Stimulation
Venturing into the world of vagus nerve stimulation (VNS) unveils exciting connections between the body’s electrical impulses and overall well-being.
Vagus Nerve and Autonomic Nervous System
The vagus nerve is a critical component of the autonomic nervous system (ANS), which oversees a vast array of involuntary bodily functions. This nerve is the main element of the parasympathetic nervous system, the part that promotes rest and digest activities, counteracting the sympathetic nervous system responsible for the body’s fight or flight responses. The vagus nerve influences the brain, heart rate, breathing, and digestion, acting as a calming force when stress levels rise.
VNS Therapy and Electrical Impulses
VNS therapy involves delivering controlled electrical impulses to the vagus nerve. By strategically stimulating this nerve, doctors aim to harness its influence over various body systems, such as modulating heart rate and respiratory patterns. Studies on VNS therapy and electrical impulses highlight its therapeutic potential for conditions where the ANS needs rebalancing, showing significant promise as a frontier in medical treatment.
Clinical Applications and Procedures
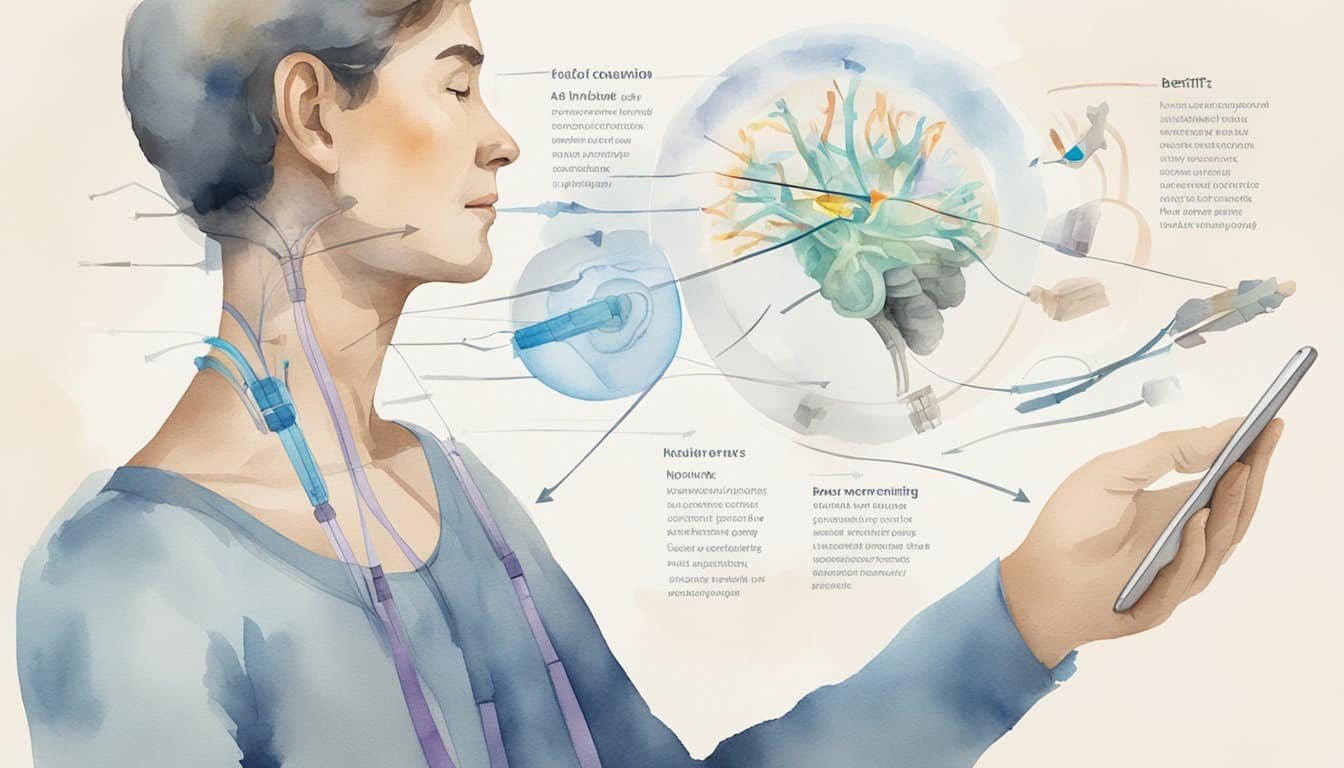
Vagus nerve stimulation (VNS) is an innovative treatment offering new hope for patients with certain chronic conditions where traditional therapies have fallen short. It involves the use of a small device that sends electrical impulses to the brain, having diverse therapeutic effects.
Conditions Treated by VNS
Vagus nerve stimulation is predominantly approved for individuals with epilepsy and treatment-resistant depression, providing relief from seizures and improving mood, respectively. Research is also exploring its potential in managing cluster headaches and migraines, aiming to decrease intensity and frequency. Advances in clinical neuroscience have opened discussions about VNS as a therapeutic option for conditions beyond the brain, including inflammatory bowel disease, rheumatoid arthritis, and possibly even Alzheimer’s disease. The technology is also being assessed for its role in sleep apnea, obesity, heart disease, and type 2 diabetes.
Overview of the clinical applications of vagus nerve stimulation
The VNS Device and Surgery
The key component of VNS therapy is the vagus nerve stimulator, a device planted under the skin of the chest. Thin wires connect it to the left vagus nerve in the neck. The procedure is typically outpatient and takes around 1 to 2 hours. The device’s settings are adjustable and tailored to the patient’s needs, sometimes requiring several follow-up visits to optimize.
Vagus nerve stimulation: from pre-clinical to clinical application: challenges and future directions
Post-Operative Care and Complications
After VNS device implantation, patients embark on a recovery phase that includes wound care and monitoring for any signs of infection or complications. The most common side-effects might include voice alterations, cough, or throat tingling during stimulation. Long-term complications are rare but can occur, and the device may require replacement every 5 to 10 years due to battery depletion.
A review of vagus nerve stimulation as a therapeutic intervention
Benefits, Risks, and Considerations
Vagus nerve stimulation (VNS) presents a beacon of hope for those struggling with certain chronic conditions, but one must tread carefully, considering both the potential for improved quality of life and the spectrum of risks involved.
Assessing the Effectiveness of VNS
When discussing the effectiveness of VNS, clinicians often focus on measurable improvements in quality of life. VNS has shown promise for conditions resistant to conventional treatment, particularly in the realm of epilepsy and depression. For instance, an increase in seizure control and a reduction in depressive symptoms are potential benefits. These gains are not always immediate and may require careful programming of the stimulator’s settings over time.
Potential Side Effects and Risks
Like any therapeutic intervention, VNS comes with a series of potential side effects and risks that must be weighed against its benefits. The side effects can range from hoarseness or throat pain to more serious concerns such as potential lead migration or device malfunction. Additionally, the surgical implantation involves risks, such as infection or complications at the incision site. The battery of the stimulator also requires periodic replacement, which means additional surgeries throughout the patient’s lifetime. These considerations are crucial, as they can impact the post-surgery recovery and overall experience with the device. The Food and Drug Administration (FDA) plays a key role in ensuring the safety of VNS devices, but patients and physicians must also work closely together to monitor for any adverse effects following the procedure.

